January 12, 2015
Clinical Integration of the Lokomat®: San Andrés Clinic, Argentina
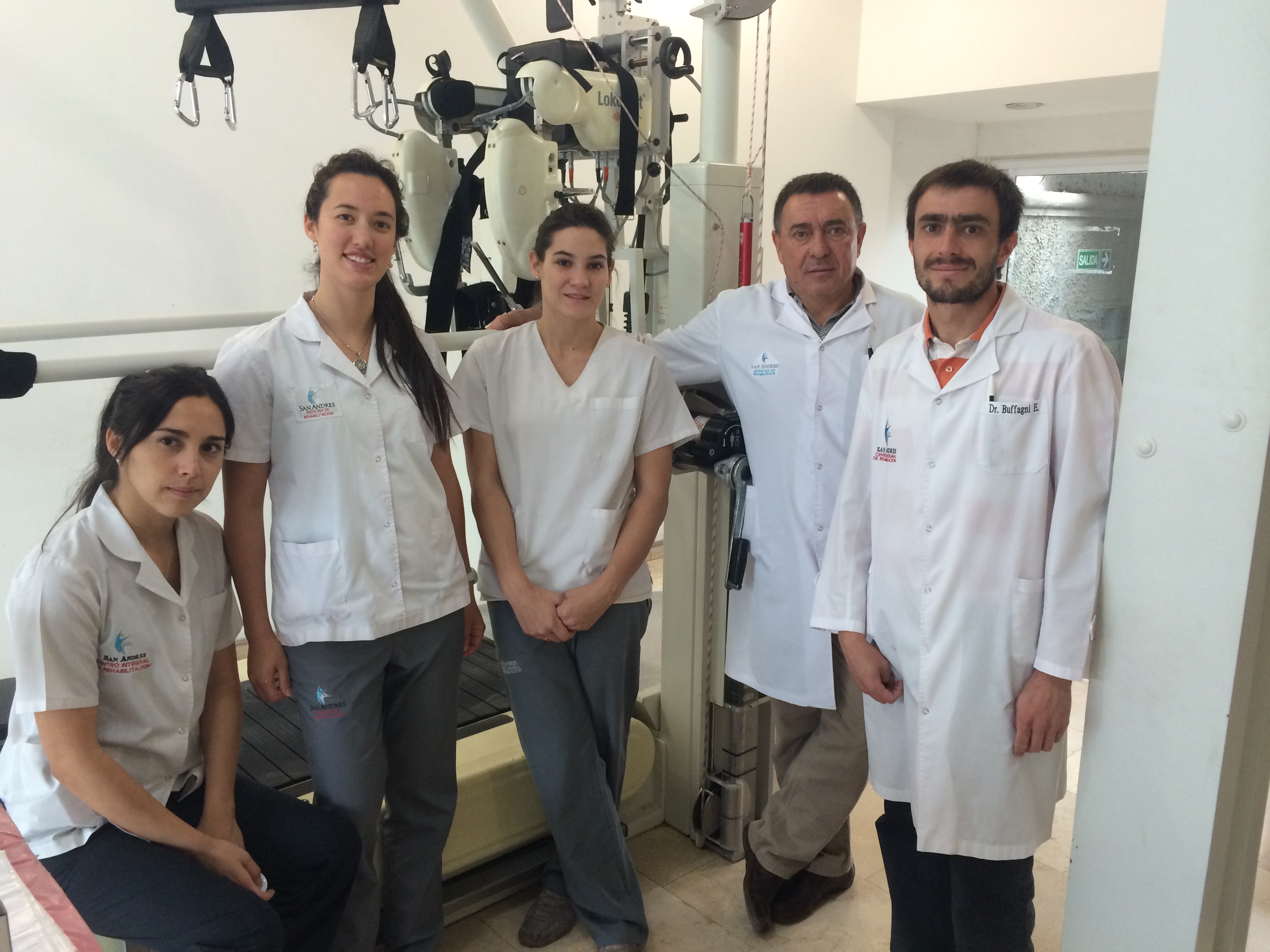
San Andrés Clinic Rehabilitation Team
Nicolás Buffagni Miralles, MD
We use the Lokomat with patients with stroke, traumatic brain injury, cerebral palsy, and with amputees. The specific reimbursement model for robotic therapy allows us to promptly pay back the cost of the device, which in turn allows us to pursue other robotic therapy devices. Lokomat therapy is provided in addition to conventional rehabilitation and clear inclusion criteria are defined.
Here we describe our clinical setting and hope that it serves as an example to support other clinics that also work with the Lokomat.
Patient Group
We use the adult module of the Lokomat with patients after stroke, traumatic brain injury, cerebral palsy and also with amputees.
We have many patients in an acute phase and we use the Lokomat, as well as the Erigo and ArmeoSpring, intensively in the early phase of rehabilitation.
Prescription: Inclusion Criteria
Our clinic is often fully booked. Thus, the inclusion criteria is rather a prioritization criteria based on which patients would benefit the most from using the Lokomat. Priority is given as follows.
- Normally, when a patient comes to our clinic, he first receives Erigo therapy because early on, acute patients who come in are severely affected and the Erigo is the first choice in providing them early rehabilitation.
Patients with a higher recovery potential. For instance, a stroke patient has priority over a complete spinal cord injury (SCI) patient. - Acute patients have priority over chronic patients.
- Younger patients have priority over older patients.
Then, those who improve move on to Lokomat therapy—especially when independent gait is a realistic therapy goal. The criteria to move on to Lokomat therapy in our center are:
- Cephalic and trunk control.
- Stable orthostatic system so the patient is stable and safe. This means the patient has no vascular disorders which imply a risk.
- Minimum cognitive status so that the patient is not aggressive and cooperates with the treatment.
Besides neurological patients, amputees also receive Lokomat therapy in our clinic. The criteria for this patient group is to be able to provide the patient a functional gait with the Lokomat so that his walking ability improves outside of the Lokomat. This means, that the setup and adjustments in the Lokomat will allow us to provide the patient a “nice” walk despite his asymmetries, prosthesis, etc. Also, Lokomat therapy must not be risky for amputee patients. The risks which we mainly consider with amputee patients are:
- Sensibility of the stump: the patient should not have hyper sensibility, especially at the contact-points with the orthopedic equipment.
- Level of amputation: it should be possible to align the patient properly during setup.
- Vascular disorders: the patient should not have associated vascular disorders.
Duration and Frequency of Lokomat® Sessions
Most patients receive Lokomat therapy three times per week, which is the frequency we aim for. When it is not possible to carry out three sessions, we do two sessions a week.
Patients are scheduled to train on the Lokomat every hour. The patient walks between 20 and 40 minutes. This variation depends mainly on whether the patient requires special care, such as hygienic considerations, which requires longer prep time.
Our goal is to provide the most frequent and intense treatment possible without overloading the patient. If the patient tolerates well five sessions per week and the schedule allows it, then we organize it accordingly. However, based on the results from our patients and experience, three sessions per week is well tolerated.
The overall duration of the Lokomat treatment varies between three months and one year. This depends on (a) the results obtained and potential to continue improving and (b) the treatment duration authorized by the patient’s insurance.
Recovery potential: The goal is always that the patient improve as much as possible. We stop Lokomat therapy when the team considers that the maximum recovery has already been reached, and the patient enters a plateau phase of improvements. We have many patients and a waiting list, so we have to find a balance between promoting continuous improvement of currently treated patients and giving new patients the chance to start Lokomat therapy.
In order to evaluate the patient’s recovery potential, we consider the following.
- Time since the injury.
- Duration of the treatment (number of months since the patient started rehabilitation treatment).
- Clinical improvements observed throughout the treatment.
Patient Evaluation
We have four different types of evaluations in accordance with the patient group: stroke, SCI, TBI and amputees. We also shoot videos of the patient at the beginning and end of the treatment, as well as at intermediate points, to observe his improvements.
We have a group meeting once a week to discuss patient leaves and entries, evaluate the treatment provided by the rehabilitation physician and the kinesiologists (PTs) at the start treatment, and also to evaluate the patient’s progression at defined points. In these meetings we discuss each individual cases and determine what is the best treatment we can provide the patient. Thus, the patient is evaluated from all different perspectives.
The rehabilitation physician then makes the final decision as to whether the patient shall receive robotic treatment as a part of his rehabilitation program, and if so, which specific robotic devices will be included.

Patient training on the Lokomat.
Reasons to Include the Lokomat® as Part of the Therapy Program
In our clinic the Lokomat is an essential part of patient rehabilitation. We include it as part of the patient’s treatment because of the observed improvements in patients, related to the walking ability.
We find the Lokomat particularly useful as a tool because of the precise movements it provides the patient. It provides a continuously repeated physiological pattern, which is something that we would not be able to reproduce otherwise. Moreover, the objectivity which the Lokomat allows is very beneficial, since it is not dependent on the individual skills of the therapist to both provide the movement and observe the patient throughout the sessions.
Other Therapies Provided in Addition to Lokomat®
We have an integrated working plan which approaches the patient from all perspectives. It is very important for us that the patient is seen as a whole from all medical disciplines and not individually from each specialist. The program includes:
- Speech therapy
- Occupational therapy
- Nutrition counselor
- Robotics
- Conventional physical therapy
- Psychology
- Cognitive stimulation
- Medical treatment
- Amputee evaluation (if needed)
We also have an external medical practice with whom we work closely together, where the patients are sent when necessary (cardiologist, traumatologist, surgeon, etc.).
For gait rehabilitation, the patient also receives conventional therapy. This includes exercising with parallel bars, walking over different surfaces to stimulate sensitivity and proprioception, electrotherapy for muscle strength or for analgesia depending on the patient, walking with partial weight support through releasing weight on the arms, postural treatments, etc.
Organization: Responsible Therapy Team
In our team, 5 kinesiologists and 1 rehabilitation physician work in the robotics department.
The clinic philosophy is to work on a one-to-one therapist-to-patient basis in order to give the patient the most individualized treatment possible.
Billing and Financial Compensation of Lokomat® Therapy
Patients in Argentina have health insurance. Some patients pay privately, but this is less than 1% of our patients.
In the past, robotics was not explicitly recognized by health insurance providers, but we provided it anyway because we observed that the patients improved.
Health insurance providers have recognized, for two to three years now, the importance of robotics as part of the rehabilitation process. This means that now insurance pays for a “robotic module” in addition to conventional therapy. This module is not included in all insurance schemes, but the big ones have it. How many robotic sessions are covered by the insurance is evaluated on a patient-by-patient basis.
In-patients have no limit to the number of robotic sessions. We can give them as many as we consider appropriate. This means we start as soon as the patient enters our clinic and as often as the capacity of the clinic and patient’s condition allows us to.
Out-patients don’t have a limited number of sessions, but the procedure is different. We evaluate the patient, make a report and send it to insurance provider asking for the robotic module. We wait until we get the approval. Then we negotiate with the insurance provider the number of sessions per month and the duration (how many months) depending on the individual case. Usually, they authorize between 12 and 16 sessions of robotics per month with a duration between 3 and 12 months. After a year the “improvement curve” of the patient typically reduces and then we normally prescribe medical leave.
About us
We are a rehabilitation clinic with a team of specialists in different disciplines including various medical specialties such as neurology, psychology, internal medicine and intensive care. The team also includes an interdisciplinary team of kinesiologists, nutritionists, occupational therapists, phonoaudiologists, respiratory therapists and nurses.
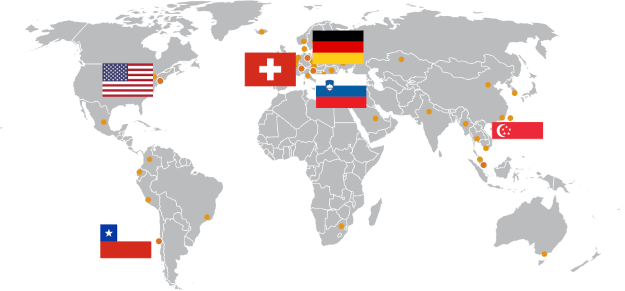
The departments and units where our patients are treated are: special care, intensive care, family support, amputees, ambulatory, stroke unit and robotics. In the robotics department we have had a Lokomat since 2009, an ArmeoSpring since 2012, a Motomed and an Erigo since 2013.
We focus on individualized programs; each patient is treated by an interdisciplinary team to best provide high-quality treatment for our patients and their families.
This clinical experience report is meant to serve as an example of how the Lokomat is integrated into the clinical setting in one individual hospital. It is not nec-essarily a standard recommendation from Hocoma.