June 9, 2016
Clinical Integration of the LokomatPro and ArmeoSpring: Centre for Advanced Rehabilitation Therapeutics (CART), Tan Tock Seng Hospital, Singapore

Lokomat Therapy, CART, Tan Tock Seng Hospital, Singapore
Dr. Karen Chua, Senior Consultant
We have the ArmeoSpring and the Lokomat integrated within our rehabilitation service through a Robowalk program and an ArmeoSpring integrated program. We have been using the Lokomat since 2008 and ArmeoSpring since 2011. Here, we describe how we integrate the robotic devices in an ambulatory outpatient rehabilitation setting.
Patient Group
The patients we treat with the Lokomat and ArmeoSpring are patients with neurological diseases. Pathologies include stroke, brain injury, cerebral palsy and spinal cord injury.
As an ambulatory outpatient rehabilitation center, our patient group varies from sub-acute to chronic.
Prescription: Inclusion Criteria
To decide whether a patient receives Lokomat therapy, first the physician and therapist evaluate the patient. If we consider Lokomat therapy suitable, we consult with the patient and his family before ultimately deciding.
The goals of Lokomat therapy depend on the condition of the patient:
- Patients requiring maximum assistance: assisted ambulation
- Patients requiring moderate assistance: improve independence in gait
- Selected patients: increased gait cycles and cardiovascular fitness training
In terms of the ArmeoSpring, we also have an inclusion criteria of proximal Upper Limb motor power of >1 for shoulder and elbow flexion on the Manual Muscle Testing (MMT) scale. The ArmeoSpring exclusion criteria includes:
- Severe cognitive/perceptual deficits
- Arm pain with a VAS score of > 5/10
- Spasticity with MAS of ≥ 3
- End stage medical conditions
Goals of ArmeoSpring therapy include the promotion of active proximal control and coordination, and building strength in the upper extremity.
Duration and Frequency of Lokomat® Sessions
We offer a RoboWalk program that includes 1 pre- and 1 post-assessment session, with 15 Lokomat sessions scheduled at a frequency of 2-3 times per week. After this period, the patient is reevaluated and it is decided whether he should undergo another 15‑session period.
The session duration is 60 minutes with actual walking time varying between 30 to 45 minutes. Balance training and over-ground gait training are also combined with Lokomat therapy.
Duration and Frequency of Armeo®Spring Sessions
Our ArmeoSpring Integrated Program includes a total of 28 training sessions comprising 16 ArmeoSpring and 12 conventional Occupational Therapy (OT) sessions. Each session is 45 minutes.
One conventional session is organized after every 4 ArmeoSpring sessions. After all 16 ArmeoSpring and conventional OT combinatory sessions are completed, the last 8 conventional Occupational Therapy sessions are completed consecutively. When the program is finished, the patient is reevaluated to decide whether to start another goal based therapeutic program. Selected patients continue maintenance therapy on ArmeoSpring.
Patient Evaluation for Lokomat® Therapy
We administer a variety of assessments pre and post Lokomat, including: the Functional Independence Measure (FIM) subscore for walk and transfers, Functional Ambulation Category (FAC), Berg Balance Scale, Modified Ashworth Scale and Lower limb Motricity Index.
For patients with Spinal Cord Injury, we also document their ASIA motor scores for Lower Limb, walking Index for Spinal Cord Injury II (WISCI-II) and the mobility subscore of the Spinal Cord Independence Measure (SCIM).
For patients who are able to walk with minimal assistance or with walking aids, the 10 m walk test and the 6-minute walk test are also documented in our functional database.
Patient Evaluation for Armeo®Spring Therapy
Outcome assessments are conducted at four fixed time points during the Integrated Program: pre-program, post‑robotic phase, post‑conventional program and at one month post‑program.
The assessments we conduct are the Upper Extremity section of the Fugl-Meyer Assessment of Motor Recovery after Stroke, the Action Research Arm Test, Grip Strength, Modified Ashworth Scale for spasticity and pain.
Organization of the Rehabilitation Team
The Rehabilitation Physician is responsible for determining the state of the patient’s medical condition and his/her fitness for therapy. Depending on the patient’s needs and goals for rehabilitation, he/she will be referred accordingly to different therapeutic services.
Following medical assessment, suitable patients are referred for individual assessments by therapists for suitability for robotic aided therapies, being guided by inclusion criteria, specific goals and patient agreement. In difficult cases, there is discussion between the rehabilitation physician and therapist on the most suitable program.

Patient treated with the Armeo®Spring at CART.
Other Therapies Provided in Addition to Robotic Rehabilitation
Patients are referred in accordance to their needs to various allied health services, including physical therapy, occupational therapy, psychology and speech therapy.
Reasons to Include the Robotic Devices as Part of Our Rehabilitation Program
- Robotic devices enable more dependent patients to engage in a larger variety and volume of rehabilitative exercises, achieving a greater range of upper and lower limb movements in a safe setup. The Lokomat allows dependent patients to experience a verticalisation experience earlier and in a safe manner with less physical effort.
- Robotic devices greatly reduce the risk of physical strain and injury to therapists and therapy assistants. In the case of gait rehabilitation of severely dependent or heavy patients with dense hemiplegia, the Lokomat saves manpower resources by allowing one therapist to conduct gait rehabilitation as opposed to 3-4 therapists that would be required if there were no Lokomat available.
- The interactive self-initiated and functional exercises and games help improve motivation. The ArmeoSpring allows active unilateral upper limb training; we also observe improved hand use, motor control and coordination, as well as an increase in strength and range of motion.
In addition to the clinical implementation of the LokomatPro and ArmeoSpring, CART also conducts research with them and other rehabilitation technologies through each robotic program’s rigorous database implementation and analysis.
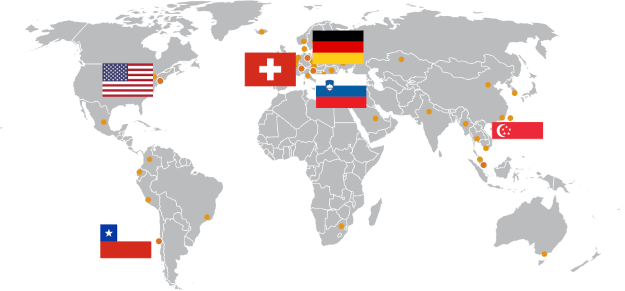
As part of the international Advanced Robotic Therapy Integrated Centers (ARTIC) network, we share our Lokomat therapy results and data onto an online database with the aim of developing guidelines and answering scientific questions with regard to the use of robotic devices in rehabilitation.
About us
TTSH is one of Singapore’s largest multi-disciplinary hospitals, with 45 clinical, allied health, and pharmacy departments, as well as 16 specialist centres. We see over 2,000 patients at our specialist clinics and approximately 460 patients at our emergency department every day.
At CART, we provide ambulatory outpatient rehabilitation consultations. Our rehabilitation programs combine regular rehabilitation therapy with innovative robotics and virtual reality technologies. Aimed at achieving goal orientated and optimal outcomes for patients, our programs are innovatively structured to increase patients’ engagement in movement retraining in a fun and interactive way.
This clinical experience report is meant to serve as an example of how the LokomatPro and ArmeoSpring are integrated into an ambulatory rehabilitation setting in a tertiary hospital. It is not necessarily a standard recommendation from Hocoma.