December 2, 2020
The Use of Lokomat®Pro in a 2 Phase Approach Treatment Period of an Acute Transverse Myelitis Patient in an Integrated Interdisciplinary Team

Santiago de Arrascaeta- Physical Therapist (Main Author), Dr Arturo Pichardo Egea, Dr. Demetrio Villa Nueva- Specialist in Biomechanics, María Alejandra Martínez Alvarez – Nutritionist, Dra. Paola Yazmín Jiménez Colín
Clinica CEREBRO, Mexico City, Mexico
We would like to share our clinical experience with a patient suffering from an acute transverse myelitis.
Diego arrived to our clinic 6 months after his diagnosis, he came in a wheelchair and he was unable to stand without any help. In Cerebro clinic, he was treated by an interdisciplinary team that included specialists in neurorehabilitation, physiotherapy, sports medicine, nutrition, psychology and biomechanics. Treatment was based on an intensive functional training on the Lokomat Pro, an upper body and core strength program and prolonged specific muscle stretching’s routines.
At the end of the treatment, our patient achieved walking without any assistance. The motivation of the patient let us to work on precise and challenging goals for each phase during the entire treatment. Having such a diverse, motivated and big team encouraged us to share the evaluations, the treatment given and the patient’s progression over more than a year.
Lokomat Pro Treatment
In accordance with progressive treatment goals, the treatment period was splitted in two phases:
- Phase 1: from March to May, 20 sessions;
- Phase 2: from May to October, 38 sessions.
Treatment included 2 sessions of robotic rehabilitation per week, each one of 40 minutes of effective gait training.
Pre-treatment / First Assessment (March 2018) : Case Information & Physical Evaluation
- Age: 15 years old
- Diagnosis: Acute Transverse Myelitis T5 with spastic paraplegia.
- First assessment in Clínica Cerebro: 6 months after his diagnosis as an outpatient.
- Relevant previous clinical interventions: Botulinum Toxin infiltrations on gastrocnemius (equinus)
Physical and Functional Evaluation (March 2018):
- Wheel-chair user
- Functional Ambulation Categories (FAC) 0/5: patient cannot walk, or needs help from 2 or more persons
- Standing position achieved with help of a familiar.
- Exhaustible clonus on both gastrocnemius, Ashworth score 2
- Sensation and mild bladder control, neuropatic intestine without control or sensation (pharma treatment)
Treatment Phase 1 (March-May 2018)
Goals
To improve:
- Range of Motion (ROM) and muscle strength in lower limbs
- Balance and postural control in standing position
- Coordination in lower limbs
- Muscle mass (also decreasing body fat mass)
Intervention :
- Intensive Home Stretching program for psoas, hamstrings, adductors and gastrocnemius.
- Gait training and functional exercises with LokomatPro.
Treatment with Lokomat (goals and intervention) :
- Challenge bilateral hip flexion and knee extension using biofeedback task-oriented activities.
- Strengthen the upper body and increasing the proprioception and recruitment of the muscles in lower limbs and core using bands to simulate the movement of a deadlift or bench press.
- The patient participation could be monitored through the picks on the lines of the biofeedback graphs
Second Assessment (May 2018): Case Information & Physical Evaluation
Physical and Functional Evaluation (May 2018)
Patient shows motor improvements, especially for gait: he is able to walk with a walker.
- Standing is achieved with the only assistance of one person holding the walker down.
- Minimum help required for dressing.
- Improvement in the sphincters control of bladder and intestine, with control at will.
Treatment Phase 2 (May- October 2018)
Goals:
To improve:
- Gait performance.
- Coordination and activation of the lower limb muscles.
- Bilateral strength of hamstrings, quadriceps and iliopsoas.
- Core strength (necessary to improve gait)
During this phase, discharge has to be prepared: starting the enrolment in sport/exercise activities is required.
Intervention similar to previous period:
- Home Stretching program for the following muscles: Psoas, Hamstrings, Adductors and Mastrocnemius (stretching 30-40 seconds 4-5 times daily).
- Isokinetic exercises for quadriceps and hamstrings to work muscle coordination at different speeds (60°- 150°degrees per second) with electrostimulation applied to ankle dorsiflexors to increase strength.
- Home Strength program which includes sit ups, lounges, lateral bridges, planks, pushups…
- Gait re-education exercises on the Lokomat and overground.
- Patient is suggested to start a strength training program at a local gym (in company of a therapist), or another sport activity he prefers.
Lokomat Intervention:
Because of the slower swing phase of the left hip, the Lokomat was used with asymmetric parameters:
- left hip with maximum extension -5 ROM and Guidance Force at 40-60%
- right hip with maximum flexion +5 ROM,
During walking, patient was pulling a resistance band to right side when left foot was on swing phase, this was done with the purpose of facilitating more proprioceptive information and challenge to the left hip by stretching and enabling the activation the abdominal muscles to help with the hip flexion as synergist.
Meanwhile, therapist watched the biofeedback graphs, and could observe the oscillation curves rising on the left hip while doing the resisted exercise.
Patient could also work with speed changes the speed using the Faster activity (1.0-2.0km/hr). Nevertheless, speed changes were not driven by visual feedback but by verbal command from the therapist.
Third Assessment (October 31, 2018): Physical Evaluation
- Patient arrives walking with a four- points cane, he is 100% independent in his daily activities and is joining Pilates lessons at his hometown
- After the assessment he was discharged and asked to come back in 6 months for re-evaluation.
Strength and Gait assessments
Strenght assessment:
During the entire treatment, a bilateral and progressive improvement of the muscular strength was observed, especially in abdominal muscles, iliopsoas, tibialis, gluteus medius and gluteus maximus. (Table 1)
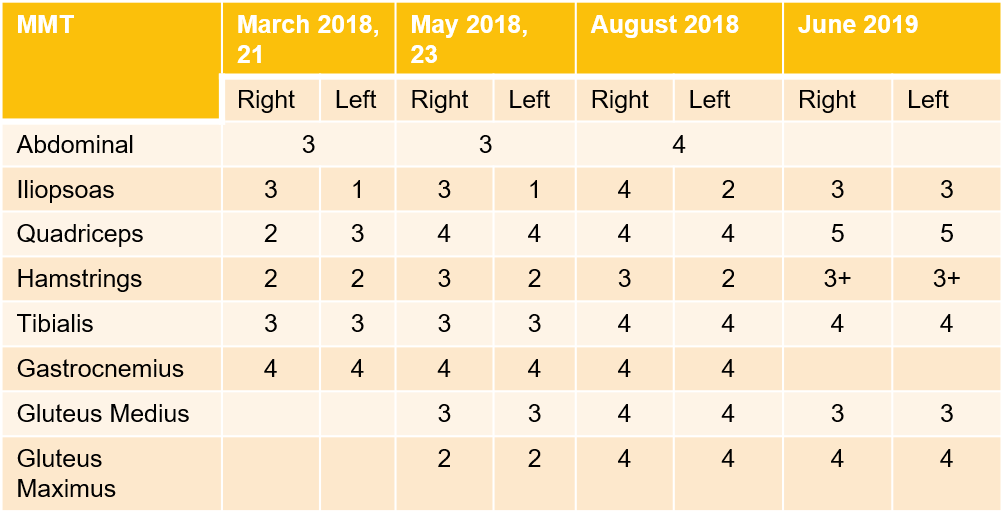
Table 1: comparison of MMT along 4 assessments
Gait Analysis
- Assessments :
- Spatio-temporal gait parameters and knee flexion-extension angles (figure 1 and 2) were analyzed
- Initial assessment in March: The patient was helped by his parents to stand, the father helped to complete the movement of the left leg while walking
- Assessment in October: The patient did the test with Canadian crutches.
- Improvements on the spatial temporal parameters compared to the assessment on March and October:
- Gait more symmetric: spatial temporal parameters for right and left more similar,
- Big improvement on the cadence and walking speed:
- Cadence (steps/min) March: NV; October: 41,98;
- Speed (m/s) March: 0,04; October: 0,18;
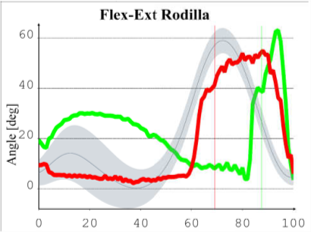
Figure 1: Knee Flexion-Extension during shoeless assisted gait (Green-right side; Red-left side; gray-range of normality)
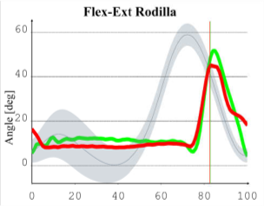
Figure 2: Knee Flexion-Extension during shoeless assisted gait (Green-rigth side; Red-left side; gray-range of normality)
To record the kinematic values was used: opto-electronic system Smart-D (BTS, Italy) and 6 camcorders infrared range with capture rate of 140 frames per second (140 Hz). To start recording the spherical markers were placed in July (15 mm diameter) of reflective material on anatomical landmarks according to protocol Short-Brain. For registration of the reaction forces used force plate model 9286BA (Kistler, USA). Conventional video was recorded at the coronal (anterior and posterior) and sagittal (right lateral view and left side). Data were processed with the Smart-Analyzer (BTS, Italy)
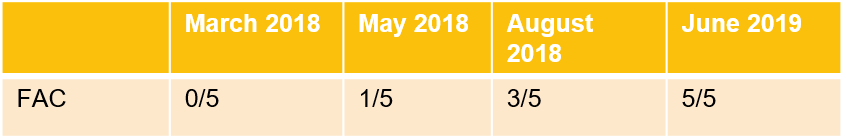
Table 3: comparison of FAC ( Functional Ambulation categories) along the 4 assessments
Follow-up (June 5, 2019)
- Re-assessment 7 months after discharge:
- Physical and Functional Assessment:
- FAC=5
- Sphincters Control = 100 %
- He walks with a cane. Cadence 63.9 steps/min. Able to go up and downstairs without any assistance.
- Physical and Functional Assessment:
- Still having therapy at home, including:
- Pilates
- Stationary bike
- Strengthening exercises
- Stretching routine
- Recommendations after the follow-up assessment:
- Continue to perform the Home Program
- Start sport activities and gym
Conclusion
The results from the team work were very satisfactory and successful, both for health professionals and for the patient. With the integration of all disciplines, all the possibilities were potentiated to enable the goal achievement.
Finally, this collaborative work must always consider the patient as the center and his interests and priorities as the best tools to achieve the drawn objectives.
About us

We are a team of specialists that includes disciplines such as neurorehabilitation, sports medicine, physiotherapy, biomechanics and nutrition. The type of patients we serve covers pathologies such as: neurological, orthopedic and sports. In CEREBRO we help our patients achieve their highest possible levels of functional independence and quality of live. Cerebro offers both upper and lower extremity rehabilitation robotics within its clinical programs in order to allow the patients to improve their motor functions through repetitive, controlled motion. CEREBRO also has a motion analysis lab to assess the functional status of the patients and measure the functional outcomes.
This clinical experience report is meant to serve as an example of how the Lokomat is integrated into one particular rehabilitation center. It is not necessarily a standard recommendation from Hocoma.