November 12, 2018
Case Report: Using the Armeo®Spring in Upper Extremity Motor Recovery Following Stroke

Erica Cirilli, MS, OTR/L
King David Center for Nursing and Rehabilitation, New York, USA
We would like to share the clinical experience we had with a patient whom we’ll call ZM. ZM had a stroke which resulted in a decreased quality of life. When ZM was first admitted to King David Center she spent most of her time in her room. She lacked the motivation to participate in recreational activities due to the severity of her limitations and overall low self-esteem. ZM began participating in occupational and physical rehabilitation to help regain her independence and increase her quality of life. Below is our case study presenting ZM’s journey throughout her rehabilitation, from her evaluation upon admission, interventions/methods used, and results post treatment. We hope that our case study will inspire other clinicians to utilize computer-based exoskeletons to enhance therapeutic outcomes.
Initial Evaluation
Patient ZM is a 62-year-old lady admitted to King David Center on 15 March 2018 following a diagnosis of cerebellar stroke/intraparenchymal hemorrhage after tPA (tissue Plasminogen Activator).
Prior Level of Function (PLOF): Our patient previously resided alone in an apartment and was independent, meaning she could do all activities of daily living (ADL). The patient did not use any adaptive equipment prior to the injury.
ZM’s cerebrovascular accident (CVA) resulted in residual deficits which severely impacted the level of occupational performance in meaningful tasks. The patient exhibited the following presentation:
- Left upper extremity hemiparesis/flaccidity (muscle weakness and hypotonicity)
- Pain in the affected extremity
- Poor trunk/postural control
- Decreased left-hand dexterity/fine motor control
- Decreased left upper extremity gross motor coordination
Manual Muscle Testing (MMT) was used in order to grossly assess the patient’s range of motion and muscle strength. ZM performed a muscle grade of 1/5 (5/5 being highest muscle grade), indicating no active range of motion even when the weight of the extremity was compensated for, although palpable muscle contraction was felt. ZM was able to provide passive range of motion within functional limits.
Table 1: Initial MMT.
|
|
Muscle Strength | AROM | PROM |
| (R) UE | 3/5 | WFL | WFL |
| (L) UE | 1/5 (flaccid/ hypotonic) | Impaired | WFL |
(R) UE: right upper extremity; (L) UE: left upper extremity; AROM: active range of motion; PROM: passive range of motion; WFL: within functional limits.
We used the Universal Pain Scale to rate the patient’s perceived level of pain (0 = no pain; 10 = highest level of pain). ZM reported 4/10 intermittent pain at rest and 8/10 constant pain during movement in the affected arm.
Table 2: Pain Scale.
| Rest | Movement | |
| (L) UE | 4/10 (intermittent) | 8/10 (constant) |
While observing her basic self-care tasks, ZM required maximum assistance for self-feeding and was completely dependent for all other basic ADLs.
Table 3: Self-care Initial Assessment (ADLs).
| Self-Feeding | MA |
| Hygiene/Grooming | TD (+) |
| Toileting | TD |
| Upper Body Dressing | TD (+) |
| Lower Body Dressing | TD |
MA: maximum assistance; TD: total dependence.
The Quality of Life Index – Stroke Version III was used to determine the patient’s subjective report of how satisfied/dissatisfied they were and important/unimportant they viewed various aspects of their life. This test was used both pre- and post-treatment to assess whether improvement altered their perception of quality of life. The QOL Index is subdivided into four categories: Health and Functioning, Social and Economic, Psychological/Spiritual, and Family. The questionnaire is scored from 0 (lowest perceived quality of life) to 30 (highest perceived quality of life).
Table 4: Quality of Life Index – Stroke Version III Pre-test.
| Categories | Score (0 – 30) |
| Health and Functioning | 8.55 |
| Social and Economic | 14.51 |
| Psychological/Spiritual | 14.92 |
| Family Support | 14.67 |
Therapy Goals
- Patient will perform self-feeding tasks with Modified Independence
- Patient will complete hygiene/grooming tasks while sitting in front of the mirror with Modified Independence
- Patient will perform toileting tasks using a standard commode and grab bars with Modified Independence
- Patient will efficiently perform upper body dressing tasks with Modified Independence
- Patient will efficiently perform lower body dressing tasks with Modified Independence
Treatment
Patient was on skilled rehab for a total of 14 weeks. The treatment included a combination of conventional occupational therapy and ArmeoSpring therapy. Armeo spring training started 7 weeks into the program and lasted for 7 weeks. ArmeoSpring therapy specifically focused on activities in the following categories: ROM (1D), movement coordination, grasping function, ROM (2D/3D), and cognitive training.
ArmeoSpring Therapy
- 5-7 times per week
- For 7 weeks
Conventional Occupational Therapy
- 5-7 times per week
- For 14 weeks
Outcome
A post-treatment assessment of ZM’s overall functional performance and muscle strength was conducted in order to see the effectiveness of the therapy program. ZM showed improvement in general muscle strength for the affected extremity (4-/5), showing that ZM’s left upper extremity muscle strength is able to withstand slight to moderate resistance against the pull of gravity.
Table 5: Discharge MMT.
| Muscle Strength | AROM | PROM | |
| (R) UE | 4-/5 | WFL | WFL |
| (L) UE | 4-/5 | WFL | WFL |
Table 6: Self-Care Discharge Assessment (ADLs).
| Self-Feeding | Modified Independent |
| Hygiene/Grooming | Modified Independent |
| Toileting | Moderate Assistance |
| Upper Body Dressing | Contact Guard Assistance (CGA) |
| Lower Body Dressing | Minimal Assistance |
As a result of upper extremity motor improvement, ZM reached two long-term therapy goals (self-feeding/hygiene and grooming) as Modified Independent (MI) and improved upper body dressing performance to contact guard assistance (CGA) from a baseline score of TD(+). The universal pain scale was re-administered post-treatment, and ZM subjectively reported less pain in the affected arm – giving a rating of 3/10 (rest) and 6/10 (during movement). ZM had an increase in grasp function and movement coordination with a 50% increase in score throughout the 7-week treatment with the Armeo Spring.
Table 7: Quality of Life Index – Stroke Version III Post-Treatment.
| Categories | Score (0 – 30) |
| Health and Functioning | 17.55 |
| Social and Economic | 18.68 |
| Psychological/Spiritual | 18.85 |
| Family Support | 20.91 |
The final outcomes for ZM’s perceived quality of life show improvement in all four subcategories. Based on this information, one can presume that an increase in functional performance and level of independence can increase one’s perceived quality of life.
Conclusion
The overall purpose of the study was to test the effectiveness of adding ArmeoSpring to conventional therapy in a patient with left hemiparesis. ZM had improvements in some of the content areas of ArmeoSpring therapy, the results suggest that conventional therapy in conjunction with ArmeoSpring therapy improve patients’ overall levels of occupational performance and therefore increase their quality of life.
About us
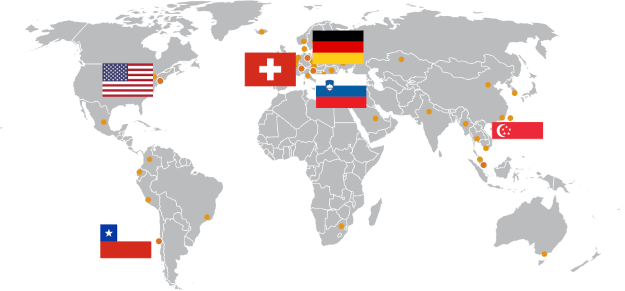
Founded in 2011, The Allure Group manages six advanced recovery centers across Brooklyn and Manhattan, NY.
The Allure Group’s holistic health centers are designed to support the growing needs of the aging population. By creating spaces that are attentive to the needs of residents when it comes to their health, comfort, culture, and quality of life, Allure’s interdisciplinary team cultivates an environment where patients can thrive. Allure is committed to providing the very latest in cutting-edge technology and treatments delivered by compassionate and skilled clinicians.