February 14, 2016
Clinical Integration of the Lokomat®: Center of Spinal Cord Injuries, Trauma Center Murnau

Lokomat Therapy Team, Trauma Center Murnau
Markus Rieger, PT and Scientific Assistant
In our center we have 2 Lokomats in a parallel setting and an Erigo which we often use as preparation for the Lokomat therapy. We provide our patients very intensive therapy, focusing on the quality of the individual sessions. To do so, we use high technology devices and also provide group therapy, including self-training sessions.
Patient Group
In our department we perform Lokomat therapy with patients with a motor incomplete spinal cord injury (SCI) classified with the American Spinal Injury Association (ASIA) Impairment Scale (AIS) C and D.
The Erigo, on the other hand, allows us to start therapy earlier, even in the intensive care unit. This is important before we can go further into Lokomat therapy, for example.
Prescription: Inclusion Criteria
All patients who (a) have no contraindications, (b) are stable for at least 30 minutes in a passive upright position and (c) have an incomplete paresis and with some function in muscles necessary for walking (ASIA C and D) are included in the training. We have many patients and therefore must prioritize this patient group since they have more potential to recover and thus have a higher chance of regaining the ability to walk independently the future.
Patients receive Lokomat therapy as soon as possible. If the patient is not yet ready for the Lokomat (based on our inclusion criteria), then we start on the Erigo and then move to Lokomat.
The patient group treated in the Erigo are those with an incomplete paresis or patients with a very high level of injury.
Duration and Frequency of Lokomat® Sessions
Lokomat therapy is performed between 3-5 times a week with our patients. Three times is the minimum because we believe in providing intensive treatment.
Each Lokomat session lasts 60 minutes including setup time. Depending on the patient’s ability to help getting the harness on (e.g. to stand up) the resulting walking time is about 30-45 minutes.
After 3 weeks of Lokomat therapy, the patients are re-assessed. If functional improvements are seen the patient continuous with Lokomat therapy. Conversely, if there are no visible improvements then we normally proceed with other techniques, such as functional electrical stimulation, physiotherapy on neurophysiological criteria, standing training and medical training therapy.
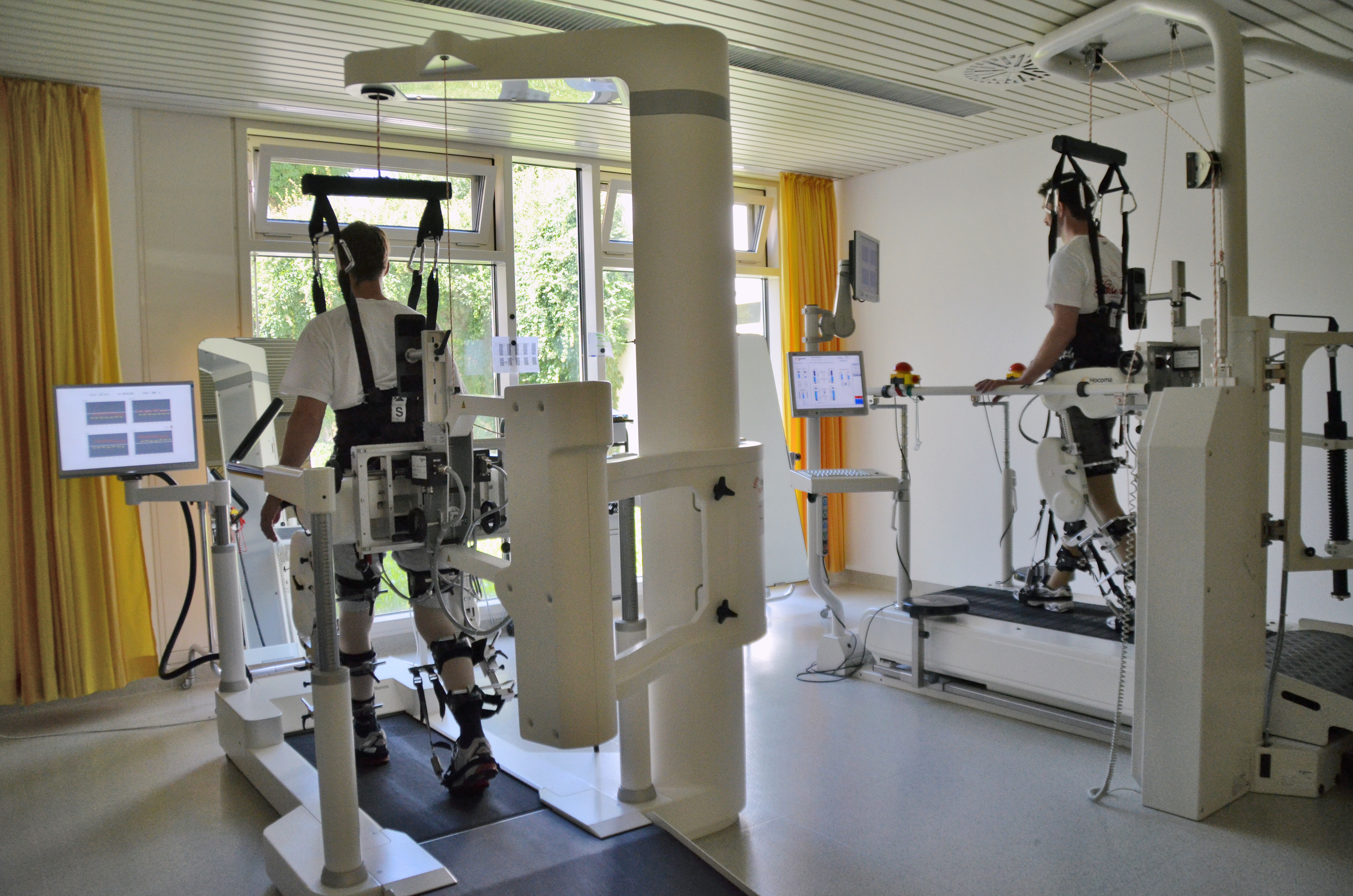
Patients treated with the Lokomats at Trauma Center Murnau.
Patient Evaluation
A therapist checks for all information (about the physical status of the patient) for our specific medical finding created for the Lokomat, which includes the following assessments:
- Muscle function test (MFT)
- Ashworth test (MAS)
- Walking assessments (WISCI-II, TUG, 10 m, 6-min walking test)
- Passive standing with tilt table >30 min
- Orthopedic status (ROM of hip, knee and ankle joint).

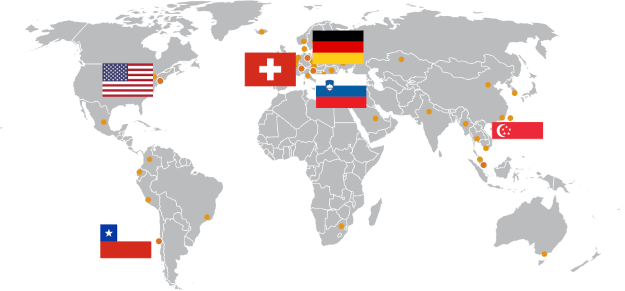
Trauma Center Murnau.
Organization: Responsible Therapy Team
All together we are 20 therapists: 19 physiotherapists and 1 sport therapist. A team of six therapists is responsible for Lokomat training.
Our Lokomats run every day from 8 a.m. to 4 p.m.
We have two systems running simultaneously with one to two therapists. To get a good workload and so the therapist has enough time to adjust the patient’s parameters and give supervision, every session starts 30 minutes after the previous one.
Other Therapies Provided in Addition to Lokomat®
We provide patients a combination of therapies adjusted to their individual needs including:
- Physiotherapy based on neurophysiological criteria (on a one-to-one basis)
- Swimming
- Standing training
- Medical training therapy (MTT)
- Wheelchair training and sports therapy
- Functional electrical stimulation (FES)
Lokomat training is done in a parallel setting. Some of our treatments are done in groups and some individually. We also offer patients additional hours of therapy per day by having self-training programs in a room together with other patients. In such programs, the situation is similar to going to a gym: we show the patient the first time the exercises and then he can come by himself and do them.
Reasons to Include the Erigo® and the Lokomat® as Part of the Therapy Program
The main goal is the recovery of the lower extremity with the end goal of standing and walking with or without aid. If spasticity is limiting the muscle function, we try to reduce it first with repetitive motion either manually or with the Motomed as preparation for the Lokomat. Whenever possible, the patient does the mobilization by himself, i.e. in our self-training room. If the patient is already able to walk, we use the Lokomat with low support of the orthosis (low guidance force values) so that the patient is able to walk for a longer time

Billing and Financial Compensation of Lokomat® Therapy
The costs of inpatient training are included in the daily rate paid by the health insurance. Outpatients pay 145€ per session.
About us
The BG Unfallklinik Murnau is a trauma center which includes a department of 100 beds for patients with a spinal cord injury. Our department is responsible for both the acute phase subsequent to injury, and also the follow-up rehabilitation and long-term care of spinal cord injured patients.
The acute phase comprises the surgical treatment of injuries and stabilization of organ functions. It is followed by transition to the rehabilitation phase.
During rehabilitation, the paraplegic patient will learn to become as independent as possible for her/his level of paralysis. This is achieved in close cooperation with physiotherapists, occupational therapists and instructors for physical education.
Another key focus of our department is the life-long follow-up care which is aimed at preventing complications associated with paralysis, and should help to recognize and treat problems at an early stage.
Therefore, check-up examinations at regular intervals are required with regard to surgery, orthopedics, urology and partly neurology.
This clinical experience report is meant to serve as an example of how the Lokomat and Erigo are integrated into one particular rehabilitation center. It is not necessarily a standard recommendation from Hocoma.